Revista
Predictable treatment of peri-implantitis by using Er:YAG laser micro-explosion. A case report
Atsuhiko Yamamoto, DDS, PhD
Lecturer, The Japan Institute for Advanced Dental Studies (JIADS), Osaka and Tokyo, Japan; President, Perio-Implant Hospital AUTIS, Osaka, Japan
With the rapid advancement of implant dentistry, many complications have been reported in recent years. One of the most serious and frequent of which is peri-implantitis. Numerous articles have discussed risk factors of peri-implantitis as well as ideas to prevent it, however predictable therapy had not yet been developed. Over the years, research has suggested that rough implant surfaces improve the osseointegration of implants. This in turn resulted in implant companies shifting their implant surfaces to have this rougher characteristic. This roughness, however also provided a favorable medium for bacteria once the surface was exposed to the oral environment. When grafting is indicated after bone resorption around an implant, it is extremely difficult to disinfect the surface, thus making the success of the grafting procedure slim. In order to regain the osseointegration, the contaminated surface must be completely removed. The Er:YAG laser is the only equipment to allow this to be accomplished. This reports revolutionary and predictable therapy for peri-implantitis using the Er:YAG laser. The implant surface is irradiated utilizing this laser. Accompanied with water micro-explosions, the Er:YAG laser decontaminates the rough titanium oxide surface of the implant and does so without causing a harmful increase in temperature (Figure 1). Animal research has proved its efficacy to restore osseointegration. In addition, our clinical cases with favorable bone regeneration around the implant body further reveals evidence of this innovative and predictable peri-implantitis therapy.
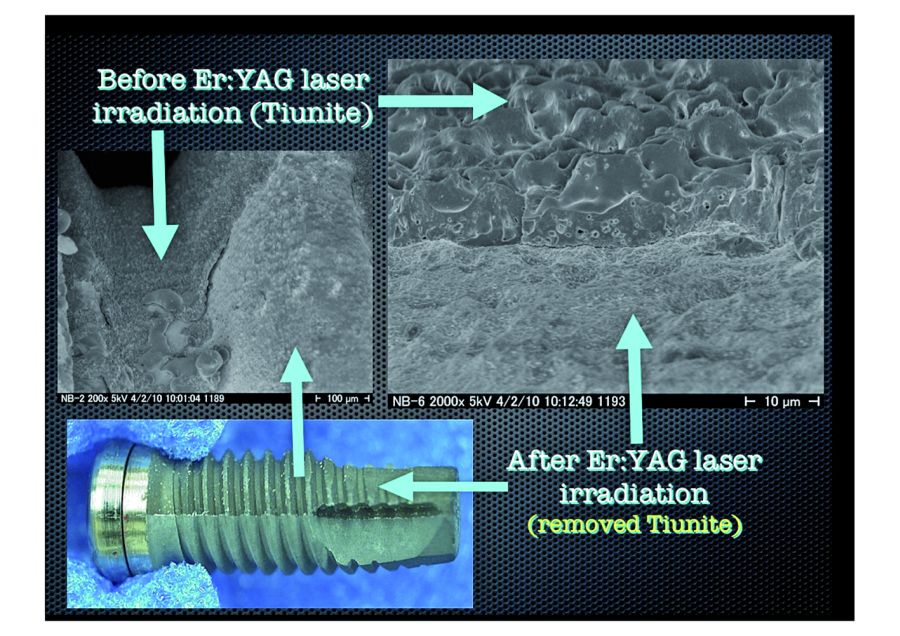 1.Phase Contrast Electron Micrographs. TiUnite layer has been completely stripped away with micro-explosions. Newly exposed surface has not been melted or otherwise deformed by the heating effect of laser irradiation.
1.Phase Contrast Electron Micrographs. TiUnite layer has been completely stripped away with micro-explosions. Newly exposed surface has not been melted or otherwise deformed by the heating effect of laser irradiation.
Clinical case
The following clinical case illustrates the use of an Er:YAG laser to treat a patient with peri-implantitis: The patient was an 81-year-old female. In September 2006, she received 9 implants in the following tooth sites: numbers 31, and 30 (lower right); 18, 19, 20, 21, and 22, (lower left); and number 11 (upper left). After 4 months, provisional restorations were made and installed. And six months later, final restorations were installed. After 5 years, the patient complained of swelling around the implants.
An x ray examination showed considerable resorption around the implants in the region of the first molar. We removed the super-structure and found that the implants was not loose. There are two types of implant periodontal inflammation: perimucositis, where the inflammation is limited to the mucosal membrane; and peri-implantitis, where the inflammation goes all the way to the bone.
This is a case of peri-implantitis. And examination determined that this was a CIST (Cumulative Interceptive Supportive Therapy) class D (PD>5mm, BOP+,Bone loss >2mm) case, an we treated periimplantitis with Er:YAG laser irradiation. After giving the patient a local anesthetic (2% xylocaine), the upper portion of the tooth socket was surgically opened and peeled away. Although the implants were not loose, considerable bone resorption and granulated soft tissue (Figure 2a).
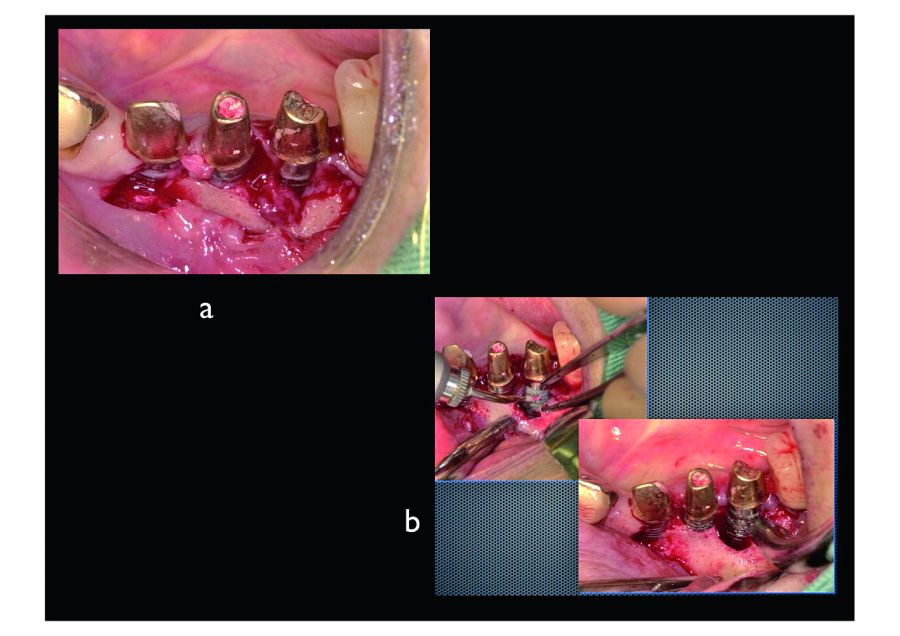 2. The key to removing contaminated granulation tissue with an Er:YAG laser is not to irradiate the granulation tissue itself but to irradiate the layer where the granulation tissue and healthy bone tissue meet. In this way the contaminated granulation tissue can be removed in a single mass. After removing the granulation tissue, we stripped away and sterilized a layer of the contaminated TiUnite surface.
2. The key to removing contaminated granulation tissue with an Er:YAG laser is not to irradiate the granulation tissue itself but to irradiate the layer where the granulation tissue and healthy bone tissue meet. In this way the contaminated granulation tissue can be removed in a single mass. After removing the granulation tissue, we stripped away and sterilized a layer of the contaminated TiUnite surface.
First the infected granulation tissue was ablated and removed by laser irradiation using a PS600T tip at 50 mJ power and 20 pps, with 5 cc per minute sterilized water spray. Granulation tissue is normally removed with a curette, but bleeding prevents the doctor from having a clear view of the treatment area when using a curette. In contrast, the Er:YAG laser with water spray eliminates this problem. The application of spray and the micro-explosions caused by the laser light hitting the water keep the treatment area clearly visible. After removing the infected granulation tissue, the contaminated implant surface was sterilized by ablating a layer of TiUnite. A PS600T tip (the flat quartz tip tapers from 600 μm in the upper part to 400 μm in the lower part), was lightly guided over the surface at 50 mJ power and 20 pps with 5 cc per minute water spray.
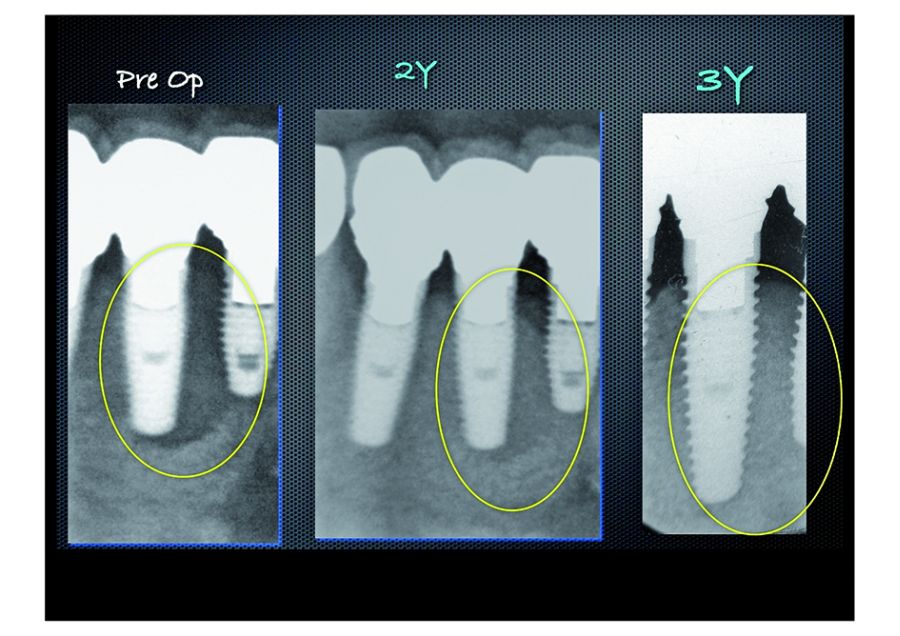 This x-ray was taken 2 years and 3 years after the treatment showing stabilized bone growth.
This x-ray was taken 2 years and 3 years after the treatment showing stabilized bone growth.
A contaminated layer was stripped away by the microexplosions caused by the Er:YAG laser’s reaction with the water spray. Slightly dark grey areas could be seen on the ablated surface; this was not carbonization but rather the new titanium surface showing through (Figure 2b). As in this case, implants are usually placed more or less vertically, and when the laser is applied perpendicular to the implant, it can easily reach detailed features of the threads and thoroughly sterilize the contaminated titanium oxide layer by stripping way an even layer. After that, an autogenous bone graft was transplanted and covered with an absorbable membrane, and the site was closed in the conventional way. Figure 3 shows the X-ray taken after 2 years and the X-ray taken after 3 years. All the X-rays show a formation considered to be bone re-growth. Figure 4 shows CT scan image(bucco-lingual cross section) made 4 years after treatment. the area around the implant has stabilized.
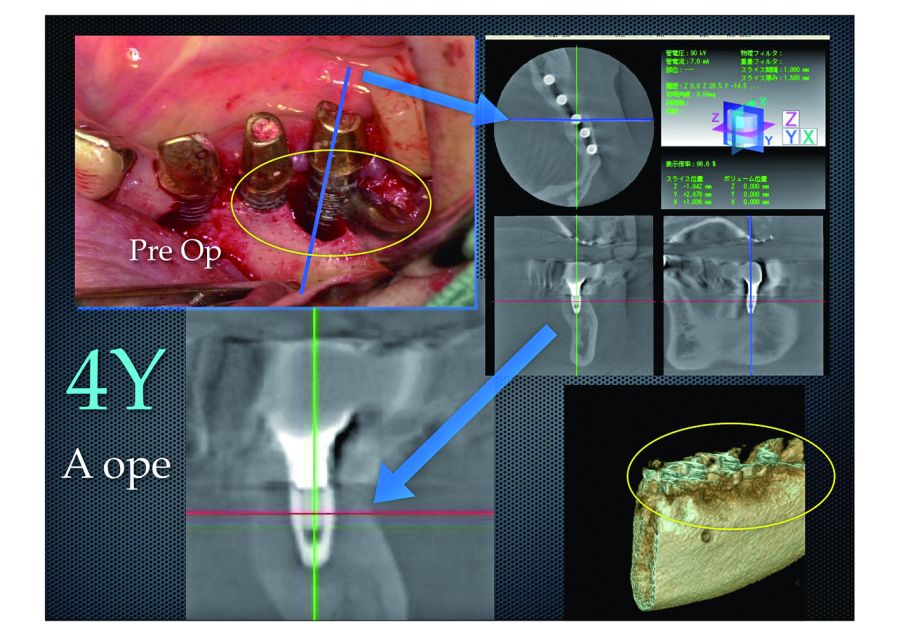 4. These are a CT scan and volume rendered image made 4 years after treatment.
4. These are a CT scan and volume rendered image made 4 years after treatment.
Compared to the photo taken when the flap was opened for treatment, the periimplantitis
has been cured and the area around the implant.
Conclusions
The micro-explosions produced by an Er:YAG laser can effectively remove the contaminated titanium oxide layer from an implant failing due to periimplantitis.
When accompanied by water spray, irradiation with the Er:YAG laser limits heating of the implant to a few degrees not enough to damage surrounding bone tissue and inhibit osseointegration. These results strongly suggest that the difficulties of treating peri-implantitis can be overcome with Er:YAG laser irradiation.
Correspondence:
Atsuhiko Yamamoto autis@silver.ocn.ne.jp

En el acto institucional “Donde nacen las ideas: historias reales desde el ecosistema de incubación empresarial”, celebrado en la sede de INCYDE, se ha visibilizado el impacto real y tangible de un modelo pionero de innovación y cohesión territorial.

La Complutense sigue siendo la Universidad más solicitada de la Comunidad de Madrid para el curso 2025-26.

Con el objetivo puesto en simplificar la labor del clínico, el Congreso SEPA Barcelona 2025, que se celebrará del 26 al 29 de noviembre, ha diseñado para esta edición especial un programa práctico y con las últimas tendencias, gracias a la participación de expertos de reconocido prestigio mundial. Así lo avanza en esta entrevista el Dr. Alberto Monje, vocal de la Junta Directiva de SEPA, quien destaca además la perspectiva multidisciplinar de este encuentro en el que tanto la utilidad de las tecnologías emergentes, el uso de inteligencia artificial y el tratamiento de las enfermedades periimplantarias serán protagonistas.

Fumar o vapear no solo afecta a los pulmones, sino que también dificulta la cicatrización, reduce el oxígeno, altera el microbioma bucal y aumenta el riesgo de infecciones como la periimplantitis: una inflamación crónica que puede hacer fracasar el implante incluso años después.

Los espacios interdentales siguen siendo los grandes olvidados por el 62% de la sociedad en su rutina diaria de higiene.
Esta formación se ha llevado a cabo en 11 ciudades de diferentes puntos de España

Existe un trastorno compulsivo denominado pagofagia, que puede provocar daños graves en el esmalte dental, fracturas y dolor de muelas y articulaciones maxilares.

La doctora Laura Pérez alerta de que el verano es una época especialmente delicada para quienes llevan ortodoncia, férula de descarga o retenedores, ya que un despiste en vacaciones puede echar por tierra meses de tratamiento.

Este curso pretende que los alumnos sean competentes en la realización de los pasos necesarios para poder llevar a término una investigación de calidad (protocolo de investigación, análisis estadístico, redacción de la publicación).

La Federación Española de Empresas de Tecnología Sanitaria ha celebrado un encuentro con sociedades científicas del ámbito médico y de la enfermería para poner en valor el Código Ético del sector respecto al marco de colaboración entre ambas partes.

