Revista
The restoration of endodontically threated posterior teeth: the full-adhesive strategy
Giovanni Tommaso Rocca
MD. Chef en clinique, Lecturer. Unite de Terapie Conservatrice et Endodontie, Section de Medecine Dentaire, Universite de Geneve.
Ivo Krejci
DMD. Professeur et Responsable de l’Unite de Terapie Conservatrice et Endodontie, Section de Medecine Dentaire, Universite de Geneve.
In the past, during millions of years, lifetime expectation of man was 30 to 40 years and one could think that evolution designed teeth for this limited period of time. However, during the last century, the lifetime expectation has drastically increased and it is now surpassing 80 years in highly developed countries. Besides challenging tooth structure as such in terms of resistance against attrition, abrasion and erosion, this development has an important impact on conservative dentistry, the goal of which is to keep teeth in the mouth of the patient during his whole life: In case a restoration is realized at the age of six or seven in a permanent tooth, it must serve for about seven to eight decades. Unfortunately, even with the best material and by using the best restorative technique, a median longevity of 70 to 80 years is not realizable today1. Thus the replacement and repair of restorations must be implemented into a modern conservative approach2. Because every replacement and even many repairs sacrifice a certain amount of nonrecoverable tooth structure, it is imperative to limit the number of retreatments to a minimum by increasing the longevity of every single restoration by highest quality and to proceed according to the rules of minimal invasivity, thus avoiding unnecessary removal of sound tooth structure. Up to now minimally invasive dentistry focused on primary restorations such as preventive resin restorations and small adhesive composite restorations. It must be stressed that the principle of minimally invasive treatment in connection with highest quality implies not only for primary restorations, but for the entire field of re-dentistry as well, thus touching large restorations on vital and, in particular, on devital teeth.
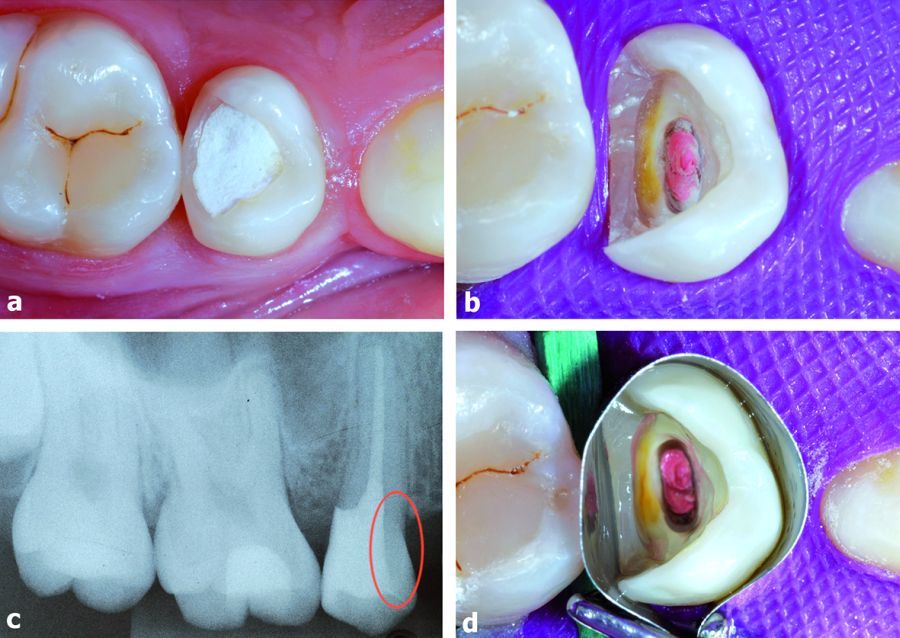 1.a) Initial view of the devitalized 1.5. The first premolar was extracted for orthodontic reasons. b) The cavity is cleaned. The distal part of the pre-endodontic resin composite is conserved to avoid a sub-gingival preparation. c) On the rx the thickness of the mesial wall is checked. d) The shiny aspect of the cavity after the application of the adhesive system.
1.a) Initial view of the devitalized 1.5. The first premolar was extracted for orthodontic reasons. b) The cavity is cleaned. The distal part of the pre-endodontic resin composite is conserved to avoid a sub-gingival preparation. c) On the rx the thickness of the mesial wall is checked. d) The shiny aspect of the cavity after the application of the adhesive system.
Minimal invasivity can only be achieved by using adhesive techniques, because adhesion assures sufficient retention without the need of tooth-destructive macroretentive and fricative elements. In addition, adhesive systems may seal the cavity thus minimizing bacterial penetration. In this perspective, the adhesive restoration of devital teeth is an excellent example how adhesion may completely change the restorative approach. With conventional techniques based on macroretention and friction, crowning of devital teeth was a must to protect the remaining tooth substance and to avoid crown fractures. To achieve sufficient macromechanical retention of the crown, a post-retained core build up had to be made. The high bonding performances reached by modern adhesive systems have gradually changed this dogma and it is now time to reconsider real indications for post and crowns.
The following cases illustrate the change in paradigm in the field of restorations of devital teeth by using direct and indirect adhesive composite techniques without radicular posts, thus avoiding more destructive restorative procedures.
Case 1. Direct composite technique
The first case is a 20 years-old woman who presented a devitalized maxillary right second premolar (tooth 1.5) with a large occluso-distal provisional restoration (Figure 1a). During the preliminary steps of the endodontic phase, the cavity was first cleaned and the pulpal tissue was removed. Then, a pre-endodontic composite resin wall was bonded on the distal aspect in order to seal the cavity during the provisional phase. A special care was put in all these preliminary adhesive procedures because the subgingival portion of that resin wall is often left in place for the definitive restoration. Once filled the root canal with gutta-percha and cement, the cavity is cleaned with a diamond bur (Figure 1b). The total loss of substance and cavity configuration are now evaluated. In a correct occlusal context, the width of the remaining walls is generally considered safe when it exceeds 1.0 to 1.5 mm, especially in the cervical part. Also the presence of weakening fissures should be detected. In the specific case of the premolar presented, the presence of a large and sound mesial wall, which protects the tooth from dramatic mesio-distal failures, allows the entire conservation of the vestibular and palatal cusps (Table 1).
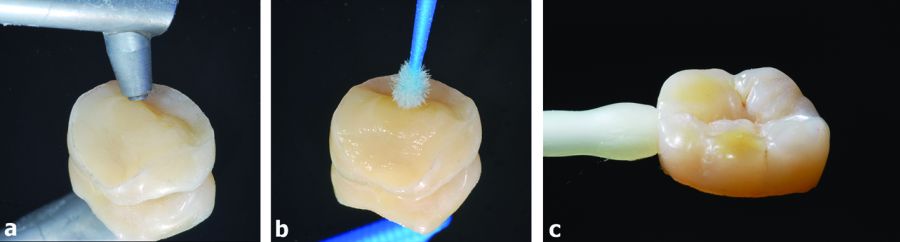
A radiographic examination must always confirm the clinical diagnosis (Figure 1c). According to the minimally invasive philosophy, the restoration by a full adhesive approach is the best choice to reinforce the system and to avoid a further loss of substance. As their quality and longevity are not essentially different, the choice of a direct or indirect technique is above all dictated by clinical feasibility. From an esthetic point of view, the possibility to conserve entirely the vestibular wall of a maxillary premolar is a great advantage. In case of pre-existing dentin discolorations, an internal bleaching with a mixture of perborate and hydrogen peroxide can be performed before the definitive restoration (Figure 4). Once the cavity isolated with a rubber-dam and a metallic matrix, adhesive procedures can be effectuated (Table 2). The distal resin composite wall is cleaned and conditioned by use of 27 microns Al2O3 sandblasting. Then, enamel and dentin are both etched with 35-37% orthophosphoric acid 10 and 30 seconds, respectively. The cavity is abundantly rinsed with water and gently dried. Dentin is then wet with an amphiphilic primer solution and well dried. Organic silane application on composite is omitted to avoid contamination of the dentinal hybrid layer. A thin layer of bonding resin is spread into the cavity, excess is removed and the resin is polymerized with a powerful LED device for 20 seconds as close as possible to the surface of the bonding layer. The next step is the application of the resin composite. The goal is to limit the resin polymerization shrinkage. To that purpose, the resin composite is progressively stratified into the cavity by 2-3 mm oblique increments, starting from the interproximal distal wall (Figures 2a-2b).
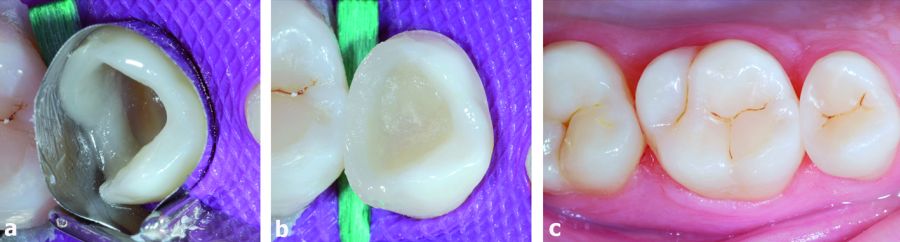 2. Stratification of the restorative resin composite. a) First, the distal interproximal wall is stratified in several increments. b) The metal matrix is removed and the occlusal part of the restoration is progressively builded-up. c) Occlusal view of the sector 1 week after.
2. Stratification of the restorative resin composite. a) First, the distal interproximal wall is stratified in several increments. b) The metal matrix is removed and the occlusal part of the restoration is progressively builded-up. c) Occlusal view of the sector 1 week after.
Each layer is polymerized for 40 seconds with the LED lamp. Then, restoration is finished and polished with silicone points and fine abrasive disks. A final touch of polymerization under glycerin gel avoids any oxygen-inhibition layers. Finally, rubber-dam is removed and occlusion is checked and eventually adjusted (Figure 2c).
Case 1. Indirect technique: the endocrown
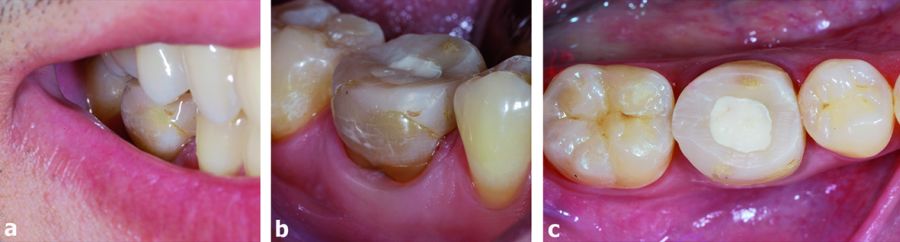 3. Vestibular and occlusal aspect of the 4.6. When the patient smiles, the esthetic aspect of the devitalized tooth is lightly grayish in the cervical part.
3. Vestibular and occlusal aspect of the 4.6. When the patient smiles, the esthetic aspect of the devitalized tooth is lightly grayish in the cervical part.
The second patient is a 30 years-old man who needs to restore an endodontically treated mandibular right first molar (4.6) with a large cavity including the mesiodistal interproximal walls and a big portion of both lingual and vestibular cusps (Figures 3a-3c). The simultaneous loss of both interproximal walls associated to an endodontic cavity has been always considered by the literature as the most inconvenient cavity configuration in term of fracture risk3,4.
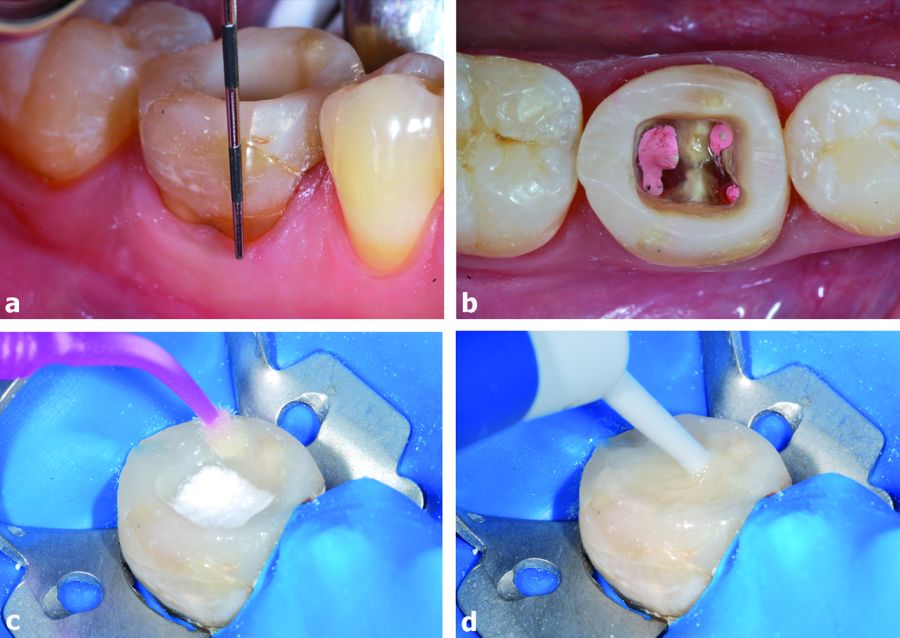 4. Tooth bleaching before the treatment. a) e b) The vestibular gingival level defines the quantity of gutta-percha that has to be removed inside the roots in the cervical part. c) A mix of sodium perborate and 3% hydrogen peroxide is inserted in the cavity. Then, a bonding resin is directly applied on the margins and polymerized. d) The cavity is easily filled with a flowable composite resin as temporary restoration and polymerized.
4. Tooth bleaching before the treatment. a) e b) The vestibular gingival level defines the quantity of gutta-percha that has to be removed inside the roots in the cervical part. c) A mix of sodium perborate and 3% hydrogen peroxide is inserted in the cavity. Then, a bonding resin is directly applied on the margins and polymerized. d) The cavity is easily filled with a flowable composite resin as temporary restoration and polymerized.
Moreover, the occlusal anatomy of the neighboring 4.7 reveals a clenching occlusal context. The set of axial and shear forces would put the vestibular and the lingual walls in high risk of catastrophic failure. Thus, a full coverage of the cusps is considered necessary to balance the occlusal forces (Table 1). At the same time, the occlusal reduction of the vestibular cusp implicates an esthetic concern. From an esthetic point of view margins of the restoration should be put in the cervical third, close to the gingival line, but this cavity configuration would mean an ulterior loss of substance. In the present case, being the inferior molar esthetic needs moderate, margins of the restoration were placed in the middle of the vestibular face at 2-3 mm from the occlusal plane. An internal bleaching of the tooth was programmed before the treatment to reach a good esthetic aspect of the remaining vestibular wall (Figures 4a-4d).
 5. The preparation of the cavity for the indirect restoration. a) After 1 week the dental dyscromia is reduced. The tooth is ready to be prepared. b) Old composite is removed and the cusps are reduced 2-3 mm. c) Cavity is isolated and adhesively treated. A hybrid composite resin is applied in the mesial and distal boxes to relocate margins occlusally. The use of a transparent shade in the first part of the pulp chamber facilitates the detection of the root canals in case of endodontic reintervention. d) Lingual and vestibular enamel is refurbished. All dentin is covered by a thin layer of composite resin. The cavity is ready to be impressed.
5. The preparation of the cavity for the indirect restoration. a) After 1 week the dental dyscromia is reduced. The tooth is ready to be prepared. b) Old composite is removed and the cusps are reduced 2-3 mm. c) Cavity is isolated and adhesively treated. A hybrid composite resin is applied in the mesial and distal boxes to relocate margins occlusally. The use of a transparent shade in the first part of the pulp chamber facilitates the detection of the root canals in case of endodontic reintervention. d) Lingual and vestibular enamel is refurbished. All dentin is covered by a thin layer of composite resin. The cavity is ready to be impressed.
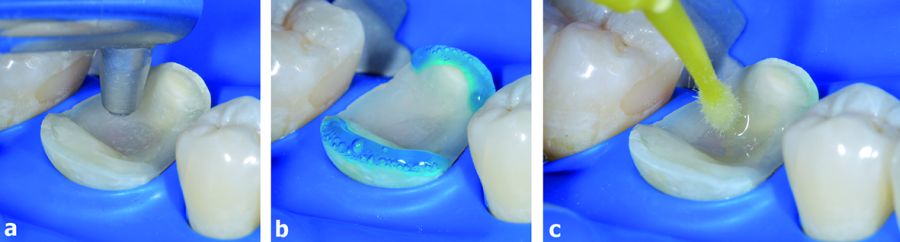
In the clinical case presented, the large amount of tissues lost due to pathology and to the endodontic treatment supports the use of an “adhesive indirect overlay restoration for devitalized teeth” or “endocrown” instead of a full crown. This technique allows for the conservation of sound dentin and, above all, peripheral enamel, maintaining the possibility to bond margins of the future restorations to it, which is known to have a beneficial effect on marginal stability5. The adhesive procedure also prevents the use of a post and a core which would be necessary in a typical crown preparation. Moreover, the adhesive cavity configuration keeps all margins of the restoration away from the periodontium, which is beneficial for hygiene and periodontal health6,7. A conventional indirect composite technique is thus accomplished, by programming two appointments8,9. During the first appointment, cavity is cut under local anesthesia in order to reach an ideal geometry. The old resin composite is removed in the interproximal regions. The vestibular and the lingual cusps are reduced in order to leave 2-3 mm from the occlusal plane (Figure 5b). Once the cavity is properly isolated (Figure 5c) an adhesive system is applied on the entire dentin and on the mesio-distal thin sub-gingival portions of enamel margins and light cured. Then, a thin composite layer is applied on dentin and into the mesial box and light cured. The aim is to fill the pulp chamber, cover all dentin and to get an ideal geometry of the cavity: correct taper, minimal undercuts, cervical margins relocated supra-gingivally and adequate interocclusal space. For that purpose, a low shrinking micro- or nano-hybrid composite is applied. The fabrication of a concavity in the middle of the pulp chamber composite will help with the positioning of the restoration during luting and improve the adhesive surface available for the future endocrown. Finishing the enamel margins with fine diamonds instruments is the last step before impression (Figure 5d).
 6. Impression and temporization of the cavity. a) An half bite tray records the cavity and the occlusion at the same time. b) The cavity is finally isolated with a layer forming glycerin gel and a soft resin temporary material is inserted into the cavity. Interproximal wedges minimize bleeding and material over-filling. c) The soft resin is then polymerized in correct occlusion.
6. Impression and temporization of the cavity. a) An half bite tray records the cavity and the occlusion at the same time. b) The cavity is finally isolated with a layer forming glycerin gel and a soft resin temporary material is inserted into the cavity. Interproximal wedges minimize bleeding and material over-filling. c) The soft resin is then polymerized in correct occlusion.
A soft lightcuring resin is applied as temporary restoration (eg Fermit, IvoclarVivadent AG, Schaan, Switzerland) (Figures 6b, 6c) The indirect restoration is then fabricated inlab. In that specific case the endocrown was milled from a CAD/CAM composite resin block (LAVA Ultimate, 3M ESPE AG, Seefeld, Germany) and then esthetically modified with a free-hand technique. During the second appointment the workpiece is tried in the mouth. The anatomy, the esthetic integration, the interproximal surface contacts and the fit of the margins are checked. Consequently, the internal surface of the indirect resin composite restoration is adhesively treated and then left under light protection.
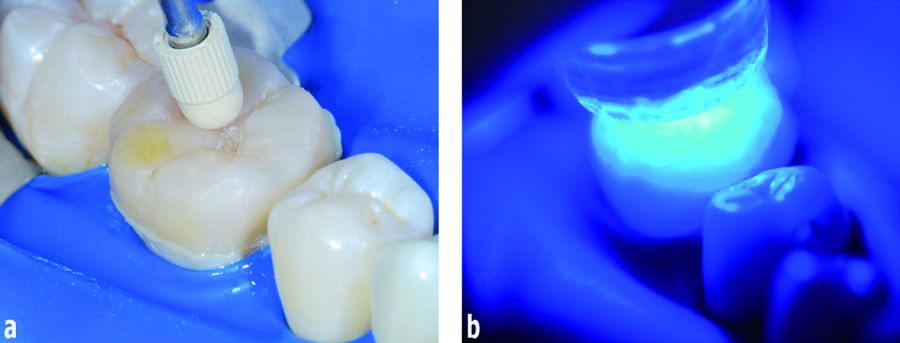
 7. The adhesive treatment of the workpiece. a) The intaglio surface is first sandblasted. b) A silane coupling agent is applied and a bonding resin is successively spread into the cavity without being pre-cured (Table 2). c) The endocrown is ready to be luted.
7. The adhesive treatment of the workpiece. a) The intaglio surface is first sandblasted. b) A silane coupling agent is applied and a bonding resin is successively spread into the cavity without being pre-cured (Table 2). c) The endocrown is ready to be luted.
(Table 2, Figures 7a-7c) The next step is the adhesive treatment of the cavity (Table 2, Figures 8a-8c). The presence of only enamel and resin composite, without exposure of dentin, facilitates the whole procedure. A conventional photopolymerizable hybrid resin composite is used as luting cement. Before the insertion into the cavity, this composite should be heated-up to a temperature of about 50°C to decrease its viscosity.
 8. The adhesive treatment of the cavity. a) Composite resin inside the cavity is sandblasted. b) Enamel is etched with H3PO4 acid. c) The bonding resin is applied and left uncured.
8. The adhesive treatment of the cavity. a) Composite resin inside the cavity is sandblasted. b) Enamel is etched with H3PO4 acid. c) The bonding resin is applied and left uncured.
Immediately thereafter, the restoration is inserted into the cavity and forced in place manually with the finger. The use of metallic plugger is contraindicated when the thickness of the restoration is fine, because it may introduce fractures. Excesses tamof luting composite at margins are removed with a probe and interproximal floss. A final push with a plastic ultrasonic tip helps to seat the restoration in its final position (Figure 9a).
 9. Luting of the endocrown. a) A thin layer of a pre-heated restorative composite resin is used as luting cement and spread into the cavity. Then, the restoration is forced in place manually and then with the help of ultrasonic energy. Excess of luting composite at the margins are removed with a probe and interproximal floss. b) The full polymerization of the endocrown is achieved with a high-power (at least 1000 mW) LED lamp for 3X90sec. in contact with the restoration.
9. Luting of the endocrown. a) A thin layer of a pre-heated restorative composite resin is used as luting cement and spread into the cavity. Then, the restoration is forced in place manually and then with the help of ultrasonic energy. Excess of luting composite at the margins are removed with a probe and interproximal floss. b) The full polymerization of the endocrown is achieved with a high-power (at least 1000 mW) LED lamp for 3X90sec. in contact with the restoration.
A first light polymerization with a high power LED unit which serves to fix the surface of the luting composite is performed for 5 s per surface. Then full polymerization in contact with the irradiated surface is achieved by light curing for at least 90 s per surface (Figure 9b). Any composite excess is subsequently removed with fine diamonds and re-polished with flexible discs or silicone points with slight pressure. A layer of glycerine gel is finally applied over the entire surface of the restored tooth and the luting composite is cured for 5 s per surface through this gel to eliminate the oxygen inhibition layer on the surface of the luting composite, if still present. Finally, rubber dam is removed and occlusion is checked (Figure 10).
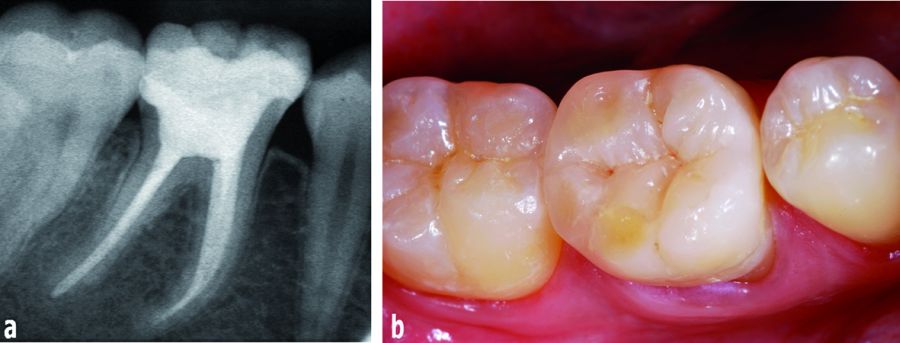 10. The radiographic (a) and clinical (b) aspect of the endocrown restoration one week after the luting.
10. The radiographic (a) and clinical (b) aspect of the endocrown restoration one week after the luting.
Conclusions
Recently, the restoration of endodontically treated teeth with adhesive techniques has been advocated both in the root and in the crown to prevent further loss of sound tissues as adhesion ensures sufficient material retention without needing an aggressive macroretentive preparation10-12. In particular, the use of bonded overlays like endocrowns for the coronal restoration of an ETT is growing against classical full-crown restorations. Reason for this change of paradigm is a more conservative approach, which preserves tooth tissues and allows re-intervention in case of failure. Furthermore, endocrowns eliminate many technical steps during the fabrication - such as post cementation, core fabrication, temporary crown and potential crown lengthening, which increase treatment time and costs. All these intermediary stages may also favor bacterial infiltration and cause endodontic re-infection. Different materials can be used to fabricate an endocrown like feldsphatic and glass-ceramic, hybrid composite and the newest CAD/CAM ceramic and composite blocks. Scientific literature is still not clear about which material is best indicated for such restorations. The authors prefer micro-hybrid composite resins - lab-made or in the form of CAD/CAM blocks - claiming their stress absorbing properties and their practical benefits like the possibility to modify and repair the surface easily13. Lithium-disilicate reinforced glass-ceramics (e.g. IPS e.max Press and CAD, Ivoclar, Schaan-Liechstenstein) may be alternatives to this concept above all for esthetic reasons. Several in-vitro studies and some in-vivo trials have confirmed the validity of this adhesive approach, especially for molars10,14-19. By relying on adhesion, no radicular posts are necessary any more on molars and at the present moment it is difficult to decide if posts are necessary on premolars and front teeth. If yes, they may only be considered in case of extremely destructed teeth. Consequently, in many instances, restoration of devital teeth may follow the same principles as the restoration of vital teeth20.
Photos copyright:
Figures 1 and 2 with the courtesy of GT. Rocca, I. Krejci, “Restaurations adhésives pour dent dépulpée. L’alternative au tout couronne”. Réalités Cliniques 2011(1)25-31.
1. Goldstein GR. The longevity of direct and indirect posterior restorations is uncertain and may be affected by a number of dentist-, patient-, and material-related factors. J Evid Based Dent Pract 2010;10:30-31.
2. Ericson D, Kidd E, McComb D, Mjör I, Noack MJ. Minimally Invasive Dentistry - concepts and techniques in cardiology. Oral Health Prev Dent 2003;1:59-72.
3. Reeh ES, Messer HH, Douglas WH. Reduction in tooth stiffness as a result of endodontic and restorative procedures J Endod 1989;15:512-6.
4. Panitvisai P, Messer HH. Cuspal deflection in molars in relation to endodontic and restorative procedures. J Endod 1995;21:57-61.
5. Pashley DH, Tay FR, Breschi L, Tjäderhane L, Carvalho RM, Carrilho M & Tezvergil-Mutluay. A State of the art etch-and-rinse adhesives. Dent Mater 2011;27:1-16.
6. Dietschi D, Bouillaguet S. Restoration of the Endodontically Treated Tooth In: Cohen S, Hargreaves KM (eds) Pathways of the pulp. St. Louis, Mo : Elsevier Mosby, 2006;777-807.
7. Koth DL. Full crown restorations and gingival inflammation in a controlled population. The Journal of prosthetic dentistry 1982;48:681-685.
8. Rocca GT, Krejci I. Bonded indirect restorations for posterior teeth: from cavity preparation to provisionalization. Quintessence International 2007;38:371-379.
9. Rocca GT, Krejci I. Bonded indirect restorations for posterior teeth: the luting appointment. Quintessence International 2007;38:543-553.
10. Krejci I, Duc O, Dietschi D, de Campos E. Marginal adaptation, retention and fracture resistance of adhesive composite restorations on devital teeth with and without posts. Operative Dentistry 2003;28:127-135.
11. Mohammadi N, Kahnamoii MA, Yeganeh PK, Navimipour EJ. Effect of fiber post and cusp coverage on fracture resistance of endodontically treated maxillary premolars directly restored with composite resin. J Endod 2009;35:1428-1432.
12. Bitter K, Kielbassa AM. Post-endodontic restorations with adhesively luted fiber-reinforced composite post systems: a review. Am J Dent 2006;20:353-60.
13. Rocca GT, Bonnafous F, Rizcalla N, Krejci I. A technique to improve the esthetic aspects of CAD/CAM composite resin restorations. J Prosthet Dent 2010;104:273-275.
14. Lin C, Chang Y, Pai C. Evaluation of failure risks in ceramic restorations for endodontically treated premolar with MOD preparation. Dent Mater 2011;27:431-438.
15. Magne P, Knezevic A. Simulated fatigue resistance of composite resin versus porcelain CAD/CAM overlay restorations on endodontically treated molars. Quintessence International 2009;40:125-133.
16. Magne P, Knezevic A. Thickness of CAD-CAM composite resin overlays influences fatigue resistance of endodontically treated premolars. Dent Mater 2009;25:1264-1268. 17. Lin C, Chang Y, Pa C. Estimation of the risk of failure for an endodontically treated maxillary premolar with MODP preparation and CAD/CAM ceramic restorations. J Endod 2009;35:1391-1395.
18. Bindl A, Mörmann WH. Clinical evaluation of adhesively placed Cerec endo-crowns after 2 years -preliminary results. The Journal of Adhesive Dentistry 1999;1:255-265.
19. Bindl A, Richter B, Mormann WH. Survival of ceramic computer-aided design/manufacturing crowns bonded to preparations with reduced macroretention geometry. The International Journal of Prosthodontics 2005;18:219-224.
20. Rocca GT, Krejci I. Crown- and post-free adhesive restorations for endodontically treated posterior teeth: from direct composite to Endocrowns. Eur J Esthet Dent 2013 ;8(2):156-79.

El Consejo General de Dentistas y la Fundación Dental Española han lanzado una campaña para concienciar a los ciudadanos de la importancia de cuidar la salud oral durante las vacaciones.

El Dr. Alberto Monje, Co-Director Médico en Clínica CICOM Monje, nos detalla algúnos de los beneficios que ofrece la implementacion del flujo digital, destacando la mejora en la comunicación con el laboratorio, así como en la precisioin y exactitud de los trabajos.

El uso de alineadores invisibles ha sido ampliamente tratado en la literatura de ortodoncia; sin embargo, aún faltan revisiones sistemáticas y meta-análisis que incluyan una gama amplia de estudios de esta área de la investigación en ortodoncia. El objetivo de la presente contribución es explorar y evaluar la literatura sobre estudios de alineadores invisibles, realizados en edades tempranas de los pacientes. Nuestros resultados sugieren que los artículos disponibles a la fecha presentan en general evidencia científica moderada, independientemente del diseño del experimento. Además, en nuestro análisis exploratorio se detectó algún grado de dependencia respecto de las variables reportadas (i.e., medidas cefalométricas), cuando se testea la heterogeneidad entre estudios. Por último, independientemente de la amplia gama de condiciones diferentes incluidas en los estudios analizados, la mayoría de ellos coinciden en que el tratamiento con alineadores invisibles puede abordar eficientemente la mayoría de las maloclusiones en niños y adolescentes.

En el acto institucional “Donde nacen las ideas: historias reales desde el ecosistema de incubación empresarial”, celebrado en la sede de INCYDE, se ha visibilizado el impacto real y tangible de un modelo pionero de innovación y cohesión territorial.

La Complutense sigue siendo la Universidad más solicitada de la Comunidad de Madrid para el curso 2025-26.

Con el objetivo puesto en simplificar la labor del clínico, el Congreso SEPA Barcelona 2025, que se celebrará del 26 al 29 de noviembre, ha diseñado para esta edición especial un programa práctico y con las últimas tendencias, gracias a la participación de expertos de reconocido prestigio mundial. Así lo avanza en esta entrevista el Dr. Alberto Monje, vocal de la Junta Directiva de SEPA, quien destaca además la perspectiva multidisciplinar de este encuentro en el que tanto la utilidad de las tecnologías emergentes, el uso de inteligencia artificial y el tratamiento de las enfermedades periimplantarias serán protagonistas.

Fumar o vapear no solo afecta a los pulmones, sino que también dificulta la cicatrización, reduce el oxígeno, altera el microbioma bucal y aumenta el riesgo de infecciones como la periimplantitis: una inflamación crónica que puede hacer fracasar el implante incluso años después.

Los espacios interdentales siguen siendo los grandes olvidados por el 62% de la sociedad en su rutina diaria de higiene.
Esta formación se ha llevado a cabo en 11 ciudades de diferentes puntos de España

Existe un trastorno compulsivo denominado pagofagia, que puede provocar daños graves en el esmalte dental, fracturas y dolor de muelas y articulaciones maxilares.

